Çocuk Kalp Hastalıkları ve Cerrahisi (Pediatric Heart Diseases and Cardiac Surgery)
Çocuk Kalp Cerrahisi Platformu (Platform for Pediatric Heart Surgery)
Pediatrik Kalp Hastalıkları ve Cerrahisi
Pediatric Heart Diseases and Cardiac Surgery
VSD-PA (VSD-Pulmoner atrezi)
VSD + Pulmoner atrezi
Doç.Dr.Buğra Harmandar
Pulmonary Atresia with Ventricular Septal Defect
Pathophysiology
Pulmonary atresia with ventricular septal defect is characterized by underdevelopment of the right ventricular outflow tract with atresia of the pulmonary valve, a large VSD and overriding of the aorta. There is a wide spectrum of severity dependent on the development of the pulmonary arteries. When a large patent ductus arteriosus is associated, pulmonary atresia with VSD is managed as a severe form of Tetralogy of Fallot. In this subtype, the pulmonary arteries are usually normal in size and distribute blood to all segments of the lungs. When a small patent ductus arteriosus is present, or when there is no patent ductus arteriosus, pulmonary artery blood supply is provided partially or entirely by major aorticopulmonary collateral arteries (MAPCAs). This form of pulmonary atresia with VSD is discussed here. Intermediate forms of this cardiac anomaly exist and are approached individually depending upon the specific anatomy.
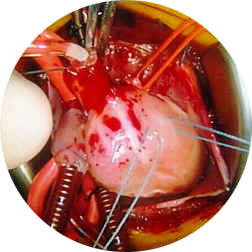
Surgical Technique
The surgical technique employed to repair pulmonary atresia with ventricular septal defect with MAPCA dependent pulmonary blood supply is variable, and depends upon individual anatomy and surgeon preference. The vast anatomic variability seen in pulmonary atresia with VSD makes the surgical approach patient specific. The ultimate goal is complete repair, achieved by constructing central pulmonary arteries from the MAPCAs, closing the VSD and establishing continuity between the right ventricle and reconstructed pulmonary arteries. Staged approach to repair, by performing sequential aorticopulmonary collateral artery unifocalization, or recruitment procedures is preferred by some surgeons. Alternatively, early single stage total repair is sometimes performed. Regardless of the approach chosen for repair of this lesion, total repair with VSD closure should proceed as early as the patient's pulmonary anatomy will allow.

Postoperative Considerations
The postoperative course following repair of pulmonary atresia with VSD and MAPCAs may vary, and depends upon individual anatomy and surgical course. Invasive monitors utilized postoperatively include arterial, central venous and left atrial catheters. An oximetric catheter is utilized to monitor cardiac output. Vasoactive infusions required for hemodynamic management might include dopamine or dobutamine, epinephrine, nitroprusside and milrinone.
Excessive postoperative bleeding can occur when extensive pulmonary artery angioplasty is required for repair. Atrioventricular conduction abnormalities are occasionally encountered since ventricular septal defect closure requires manipulation near atrioventricular conduction tissue. Atrioventricular pacing capability should be readily available. Arterial oxygen saturation and intracardiac pressures should be normal following surgery. Length of hospital stay required following repair is variable, but one to two weeks is average.
Yorumlar - Yorum Yaz








