Çocuk Kalp Hastalıkları ve Cerrahisi (Pediatric Heart Diseases and Cardiac Surgery)
Çocuk Kalp Cerrahisi Platformu (Platform for Pediatric Heart Surgery)
Pediatrik Kalp Hastalıkları ve Cerrahisi
Pediatric Heart Diseases and Cardiac Surgery
TOF - Fallot Tetralojisi
Fallot tetralojisi
6 ay 1 yaşından itibaren pulmoner arter gelişimi yeterli olanlara tam düzeltme ameliyatı yapılır. Tam düzeltme ameliyatında aort çıkımı sol ventrikül tarafında kalacak şekilde VSD kapatılır. Pulmoner stenoz giderilir.
Doç.Dr.Buğra Harmandar
Tetralogy of Fallot
Pathophysiology
Tetralogy of Fallot occurs when there is underdevelopment of the right ventricular infundibulum or conus. Ventricular septal defect, right ventricular outflow tract obstruction, right ventricular hypertrophy and overriding of the aorta are the four abnormalities classically described. Tetralogy of Fallot comprises a spectrum of severity. As the severity of right ventricular outflow tract obstruction increases, right to left shunting of blood occurs through the VSD, resulting in cyanosis. When severe right ventricular outflow tract obstruction and hypertrophy exist, hypercontractile episodes, often associated with agitation, give rise to severe right to left shunting of blood and hypercyanosis. These episodes are referred to as "tet spells".
Surgical Technique
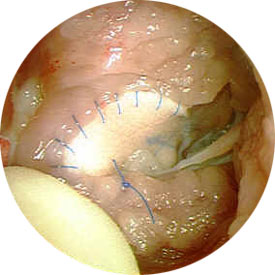
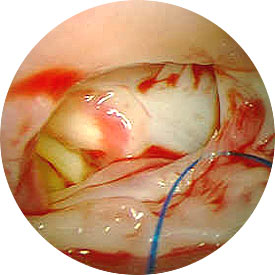
Timing of complete repair of Tetralogy of Fallot varies. Early palliation for hypercyanotic spells or severe cyanosis can be provided by a modified Blalock-Taussig shunt. Total repair of Tetralogy of Fallot requires cardiopulmonary bypass and aortic cross-clamping. Repair of this lesion can be approached via either a right atriotomy or a right ventriculotomy, depending on the degree and length of right ventricular outflow tract obstruction. Right ventricular obstruction is relieved first with resection of obstructive muscle. The ventricular septal defect is then closed with interrupted sutures. Pulmonary arterioplasty or pulmonary valvotomy is performed next, depending upon the individual needs of the patient. The integrity of the pulmonary valve annulus is spared whenever possible to maintain pulmonary valve competence. A patch across the pulmonary valve annulus (a transannular patch) is often required in order to adequately relieve right ventricular outflow tract obstruction. Following adequate rewarming, the patient is weaned from cardiopulmonary bypass. Transesophageal echocardiography is utilized to help assess adequacy of repair. Cardiopulmonary bypass time and aortic cross-clamp time required to complete repair are usually moderate in length.
Postoperative Considerations
The postoperative course following repair of Tetralogy of Fallot can be variable and depends upon the individual anatomy and surgical course. Invasive monitors utilized following surgery include arterial, central venous and left atrial catheters. An oximetric catheter is used to monitor cardiac output. Vasoactive infusions required for hemodynamic management might include dopamine or dobutamine, epinephrine, milrinone, and nitroprusside.
Some degree of right ventricular failure is nearly universal following repair of Tetralogy of Fallot. Significant resection of right ventricular muscle, coupled with pulmonary insufficiency resulting from transannular patch repair can lead to early postoperative hemodynamic instability. Since left ventricular output is dependent upon adequate transpulmonary blood flow and adequate left ventricular filling, satisfactory right ventricular function is an important determinant of postoperative hemodynamic stability. Maintaining adequate right ventricular function depends upon atrioventricular synchrony, adequate preload, and maintenance of low pulmonary vascular resistance. Inotropic support is commonly required. Normal to mildly elevated mean arterial pressure can help maintain right ventricular function and excessive afterload reduction should be avoided.
Bleeding is a potential postoperative complication and can occur in patients who have undergone extensive pulmonary artery patch angioplasty. Atrioventricular conduction abnormalities are occasionally encountered since ventricular septal defect closure requires manipulation near atrioventricular conduction tissue. Atrioventricular pacing capability should be readily available. Pleural effusion is a common postoperative complication. Prolonged chest tube drainage may be required. Arterial oxygen saturation following repair should be normal. Intracardiac pressures might reflect a higher than normal right ventricular diastolic pressure secondary to pulmonary insufficiency. In addition, central venous pressure may be elevated, indicating right ventricular failure. Intracardiac pressures usually return to normal as right ventricular performance improves. Length of hospital stay following repair of Tetralogy of Fallot is variable, but averages one to two weeks.
Yorumlar - Yorum Yaz








